In Stevens County six patients receiving care for serious illnesses were advised by their providers to transfer to Spokane in the same month. But after consultations with a palliative care provider in their community, all the patients decided to stay and have their needs met closer to home.
“Well intentioned clinicians don’t want to stop trying things. Often patients were being sent to Spokane or Seattle for more work ups or more interventions that weren’t going to do them any good,” said Pat Justis, Executive Director of the state Department of Health’s Office of Rural Health.
Justis’s office has a focus on palliative care, which provides specialized care for people with serious illness that centers on symptom and stress relief.
“The goal is to improve and sustain quality of life for the patient, loved ones, and other care companions,” said Mandy Latchaw, Office of Rural Health Program Manager. “Palliative care facilitates patient autonomy, access to information, and choice. A palliative care provider helps patients and families understand the nature of their illness, and make timely, informed decisions about care.”
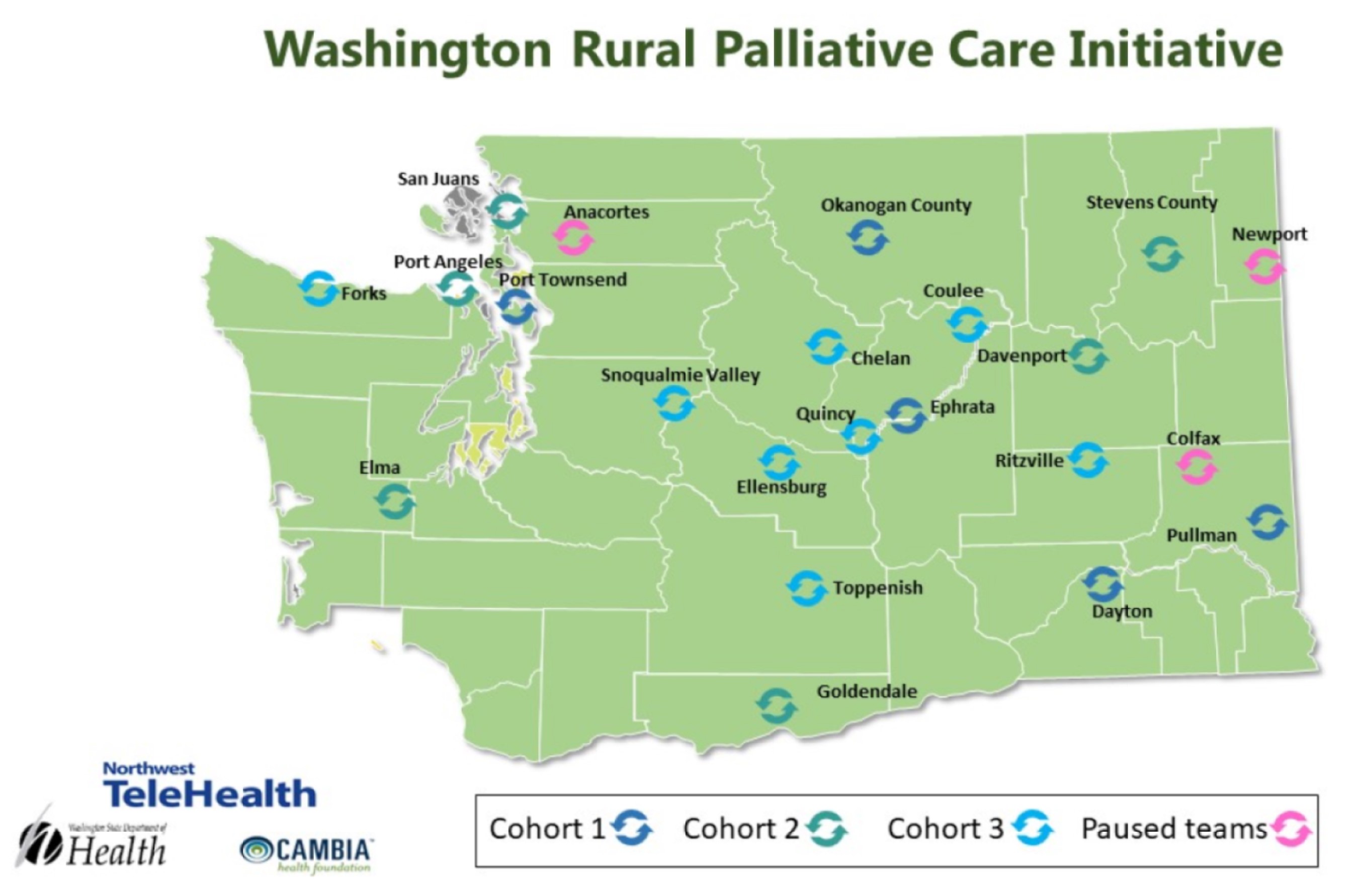
Through the Washington Rural Palliative Care Initiative, the Office of Rural Health has formed public-private partnerships with 19 rural communities.
Participants can access trainings, connect with peer mentors, and participate in roundtables and case consultations using de-identified client information. They also have leveraged the WA Portal as an access point for providers to find extensive links to resources, such as webinars, metrics, communications guidance, and clinical tools.
“The most critical need for our rural partners is just being able to find resources they need and being able to connect with each other,” Justis said. “We use WA Portal as a driver of the initiative and to enable what we do.”
Given its success, the initiative is starting to plan for sustainability and increase the percentage of rural communities using palliative care to treat their patients. Leadership intends to move past grant funding towards a self-sustaining structure that offers support for its 19 partner communities and continues to attract new communities. The team has observed that at the national level the goal is to improve the payment structure with federal and private insurers so palliative care coverage is standardized, widespread, and not limited to pediatric populations.
“National data also shows people live longer when they receive palliative care, they have a better quality of life, they have less difficulty with their symptoms, they’re more satisfied with their care, their families are more satisfied with their care, the caregivers are more satisfied with the care they’re giving, and it saves money on the total cost of care,” Justis said. “What’s not to like, as far as the outcomes go?”
See trainings and toolkits for providers working in pediatric palliative care. |